Access to Medications
At every step of the medication review and listing process, it’s crucial that Canada’s regulators and drug plans understand patient priorities in order to address gaps in arthritis treatment strategies and ensure patient needs are met. Although many Canadians have access to public or private drug insurance, the patchwork of drug plans in Canada creates inequities in access to medicines, exposes households and businesses to considerable financial burden and isolates the management of prescription drugs from other key components of the Canadian healthcare system.
Biologic medicines continue to be a growing budget pressure for public drug plans. As payors continue to spend more and more of finite health dollars on biologics—and rightly so, given their efficacy and safety—it restricts their ability to provide coverage for existing medicines and to list any new medicines on their formulary. When ACE meets public drug plan managers, we highlight that biologics are life changing for patients with inflammatory arthritis and have vastly improved the treatment and prevention of disabling diseases like rheumatoid arthritis. We acknowledge that not only do biologics have higher prices, but they also are prescribed for longer durations to younger patients in order to manage chronic diseases. These higher and growing costs continue to put pressure on public drug plans. The use of biosimilars and the savings they generate are a solution to these challenges. The savings that can be generated through broader use of biosimilars can help public drug plans provide continued coverage to arthritis patients who need a biologic to manage their disease, allow them to cover new and innovative medicines, as well as expand access to existing medications.
Amplifying patients’ needs
In order for government regulators and public drug plans to effectively review and approve new therapies and provide reimbursement access to treatment options, it is important for them to be aware of the unmet needs of arthritis patients; while at the same time, ensuring patients can afford the medicines they need.
Today, public drug plans are cost-managing formularies by restricting coverage for existing medications, delaying access to new medications and, at times, failing to address unmet treatment needs. Private insurers and pharmacy benefit managers have implemented a wide variety of cost containment programs and tools to manage plan sponsors’ drug plan costs, including case management and preferred pharmacy networks.
People living with arthritis are well aware of the gap in treatment options for many aspects of life with the disease. ACE works with people with arthritis across Canada to amplify their priorities during therapy development and throughout the regulatory approval and reimbursement access process.
Here are some of the ways ACE advocates for policies that move new medications through the most efficient review process while still upholding strict safety and efficacy standards and receive timely, equitable reimbursement coverage.
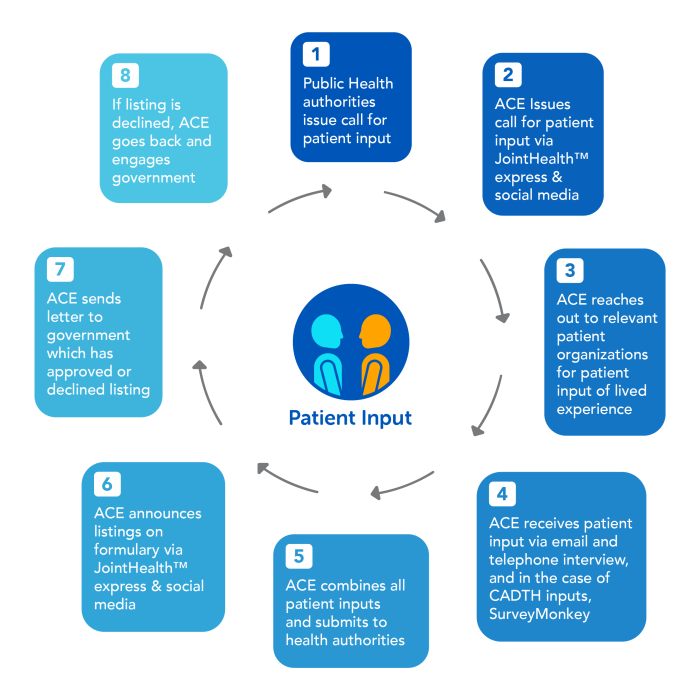
Patient input
Arthritis Consumer Experts advocates for the Canadian patient community by responding to call for patient inputs. These inputs help inform policy decisions that affect the lives of Canadians living with arthritis. ACE has delivered more patient input submissions since its inception in 1999 than any other patient group organization in Canada.
Here is the advocacy cycle ACE has pioneered and delivers year after year:
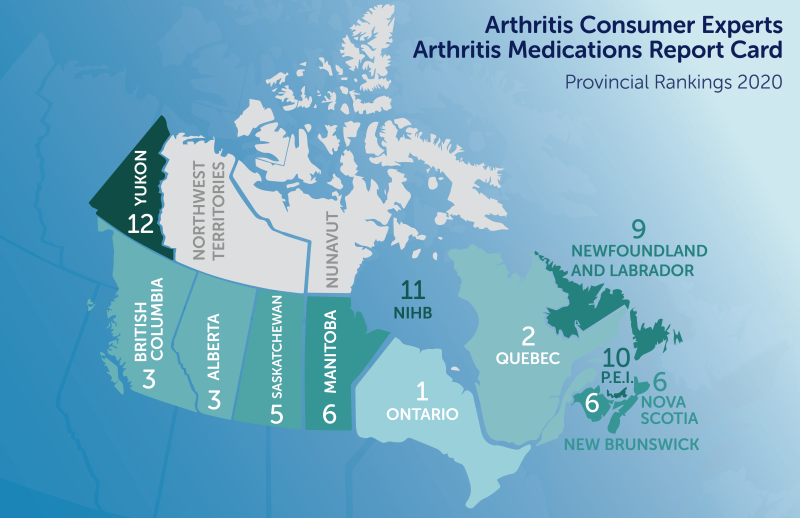
Arthritis Medications Report Card: Where does your province rank?
The Arthritis Consumer Experts Arthritis Medications Report Card has been integral to developing and implementing new arthritis health policy by making decision-making transparent and by highlighting inequity in medication reimbursement towards ensuring the best treatments are more affordable and accessible
Public drug plan policies at both the national, provincial, and territorial government levels are changing reimbursement access to treatment options for Canadians living with an inflammatory arthritis.
The Arthritis Consumer Experts Arthritis Medications Report Card is designed to help Canadians evaluate where their province ranks in terms of providing reimbursement for medications approved for inflammatory arthritis such as rheumatoid arthritis, axial spondyloarthritis, psoriatic arthritis and juvenile idiopathic arthritis.
If your province doesn’t measure up, ACE encourages you to write and speak to your elected provincial or federal representative about the lack of equitable reimbursement access and patient/physician choice in treating inflammatory forms of arthritis.
Want to get more involved?
Take action in support of expanding access to arthritis medications and contact your elected officials

Arthritis Consumer Experts
© 2000-2023